END THE WAR ON PROTEIN!! 💪🏽🏆
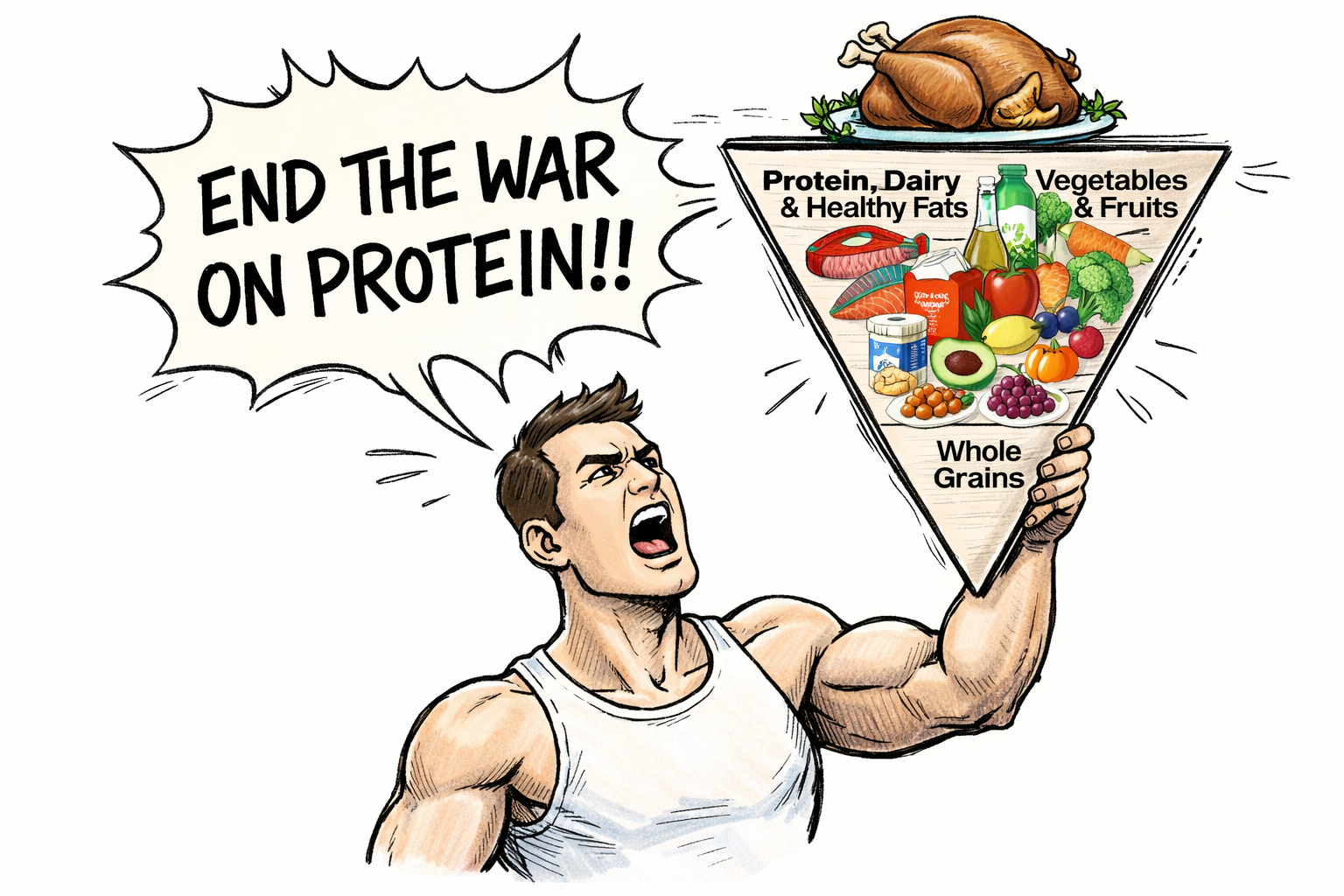
That’s the energy the new Dietary Guidelines are bringing in 2026.
And honestly? I’m not mad about the increased protein targets. This better reflects what the scientific literature has been showing for years, especially around muscle health, aging, metabolism, and weight management.
But before we talk numbers, we have to talk about the elephant in the room
Protein is everywhere. In popcorn. In soda. In candy. In chips made of chicken breast.
Welcome to the Proteinization of America!!
There are a few reasons protein has moved from a gym-bro conversation to your grandma’s grocery list:
- Protein = Satiety → Protein helps people feel full longer… and dietitians have been telling their patients to "pair carbs with protein" for decades.
- GLP-1 Medications→ With the life-changing effects of obesity medications, the way people eat is changing. People need nutrition per bite and are choosing to "optimize protein".
- Macros are trendy→ Tracking macros used to be a bodybuilder thing. Now my neighbor is telling me how many carbs he eats.
- Health halo → Adding protein to something automatically makes it appear healthier. But a pop-tart is still a pop-tart even if it has 15 grams of protein now.
So no—there isn’t a “war on protein.” If anything, protein has been winning culturally for years.
But the new Dietary Guidelines do make protein the main character in a way we haven’t seen before.
What the New Guidelines Say About Protein
The updated guidelines emphasize prioritizing protein at every meal, with a daily target of 1.2–1.6 grams per kilogram of body weight.

That’s a notable shift from the long-standing RDA of 0.8 g/kg, which many clinicians and researchers have argued is too low, especially for:
- muscle preservation
- metabolic health
- aging
- weight management
From a research perspective, this update better reflects what the literature has been saying for years.
The new guidelines included both animal and plant foods, however an obvious bias toward animal sources was apparent.
Why This Feels Like a Big Deal (Even If It’s Not New Science)
The science supporting higher protein intakes, especially for adults, has been building for a long time. Many clinicians have already been counseling patients toward higher protein patterns, particularly at breakfast (which most people struggle with).
The RDA of 0.8g/kg was established to prevent deficiency based on nitrogen-balance data. It represents the lowest intake that maintains equilibrium in most healthy adults but does not reflect the intake required to maintain optimal muscle mass or metabolic function under all conditions.
So in that sense, this change feels long overdue and evidence-aligned.
But it’s also important to say this:
👉 Americans do not have a protein deficiency.

According to the Average Intakes: Analysis of What We Eat in America, NHANES 2015-2016, adults have no problem consuming animal proteins. Besides seafood, Americans exceeed the recommended intake. So while higher targets may support specific health goals, this isn’t about fixing a widespread deficiency.
What’s Getting Less Attention: Protein Type and Balance
The guidelines acknowledge that both animal- and plant-based proteins contribute uniquely to nutrient adequacy.
Animal-source proteins provide:
- complete essential amino acids
- vitamin B12
- iron, zinc, calcium, choline
Plant-source proteins contribute:
- fiber
- folate
- magnesium
- phytonutrients
But the framing leans heavily toward animal-source foods, with minimal emphasis on plant-based foods, despite data showing numerous health benefits of plant-based diets.
What Clinicians Should Take From This
- Higher protein targets can be helpful, especially for active adults, older patients, and those focused on muscle and metabolic health
- “Protein at every meal” is a useful framing tool, but it's not life or death
- Most Americans already meet baseline protein needs
The real work is helping patients:
- distribute protein more evenly
- choose nutrient-dense, lean source and not solely rely on supplements
- pair protein with fiber and fats
- Consume a variety of protein from both animal and plant sources
Fiber: Ghosted AGAIN
Poor fiber. She should’ve gotten the spotlight. Instead, she got quick “Heyyy fiber 😍”…and then nothing.
Which is wild, because in the previous Dietary Guidelines, fiber was listed as a “dietary component of public health concern.” Why? Because more than 90% of Americans don’t meet recommended intake.

So if we actually want meaningful changes in patient outcomes, things like better glycemic control, improved lipid profiles, gut health, satiety, and cardiometabolic risk reduction, our counseling can’t only be:
“Add more protein.”
It also has to be:
👉 Build a diet that’s rich in fiber.
Because protein might be trendy. But fiber is the one doing the unglamorous work in the background… keeping the whole system running. Yay Fiber!
Up Next
I’ll break down the fat controversy and why dietitians are annoyed and consumers are confused !