Meal Plans Don't Work. Do this Instead
Don't waste your time writing meal plans (like I did)!
We’ve all had patients ask for a meal plan. But let’s be real—how many actually follow it?
Spoiler alert: NONE! (okay maybe 2%)
Meal plans fail because they assume:
❌ The patient will eat the same things every day.
❌ They won’t get bored.
❌ Life won’t get in the way. (hello parties, conferences, vacations)
Instead of wasting time on meal plans, here are 5 high-impact strategies that equip patients and actually lead to long-term change.
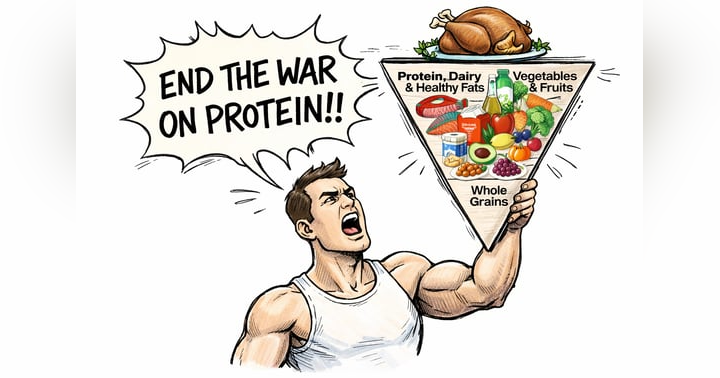
1. Teach the Plate Method Instead of Prescribing Meals
Meal plans tell people what to eat. The plate method teaches them how to eat—anywhere, anytime.
A balanced plate includes:
- Half vegetables or fruit
- A quarter protein
- A quarter whole grains or starchy vegetables
- Healthy fats for satiety
Instead of saying, “Eat chicken and quinoa,” try, “At your next meal, build your plate like this. What do you already eat that fits this approach and what could we add to make it more balanced?”
2. Focus on Meal Timing and Blood Sugar Balance
Many patients struggle with energy crashes and cravings—not because they’re eating the wrong foods, but because they’re skipping meals or eating too erratically.
Help them:
- Recognize hunger and fullness cues. Episode 33 goes into this in detail.
- Aim for regular meals and snacks every 3-5 hours
- Combine protein, fiber, and healthy fat to prevent energy dips
A simple way to start: “What time do you usually feel low energy or snacky? Let’s adjust your meal timing to prevent that.”
3. Identify Sneaky Sources of Extra Calories
Many patients don’t realize how much they consume from beverages and mindless snacking. The biggest culprits?
- Sugar-sweetened drinks (coffee shop lattes, sweet tea, soda)
- Alcohol (a glass of wine adds up fast)
- Unconscious snacking (handfuls of Goldfish, bites of a PB&J crust)
Instead of overhauling their diet, start with an easy swap: “Rather than changing your meals, let’s focus on what you drink first. What’s one simple change that feels doable?”
4. Teach Smart Grocery Shopping and Meal Prep
Most patients don’t struggle with knowing what to eat—they struggle with having it available when hunger strikes.
Encourage them to:
- Shop with a simple formula in mind (protein, vegetables, carbohydrates, and healthy fats).
- Keep easy, grab-and-go protein options on hand (Greek yogurt, rotisserie chicken, hard-boiled eggs, jerky, cheese sticks, fresh or dried druit, pre-cut veggies).
- Make your grocery cart COLORFUL!
- Focus on prepping one item at a time instead of full meals (batch cooking protein is often the easiest place to start).
Ask them, “What’s one small grocery or meal prep tweak that would make your week easier?”
5. Address Sleep and Stress Before Blaming Willpower
Sleep and stress impact hunger hormones more than any meal plan ever could.
Lack of sleep leads to increased ghrelin (the hunger hormone), stronger cravings for high-carb foods, and lower energy for movement. Chronic stress elevates cortisol, which drives fat storage and emotional eating.
Instead of immediately discussing food, start with, “Before we even talk about nutrition, how are you sleeping? No meal plan fixes exhaustion.”
TL;DR: Meal Plans Are Overrated. Behavior Change Isn’t.
Instead of handing out rigid meal plans, focus on small, sustainable shifts in:
✅ How patients eat (plate method, meal timing, food pairing)
✅ What they drink (hidden liquid calories)
✅ How they grocery shop & meal prep
✅ What’s driving their habits (sleep, stress)
Because when patients learn to make their own decisions, they stick with them.