Wound Healing and Prediabetes
This week on the podcast we covered nutrition for surgical wound healing. It was so fun interviewing another PA/RD. We discussed the key nutrients needed for optimal wound healing, when supplementation is warranted and why it is crucial that you find an opportunity to ask the patient about their eating habits. Notice how I didn't say find time .. I know that can't be found! So here are 4 opportunities for you to squeeze in a conversation about nutrition:
- While gathering supplies for dressing change: "Hey [patient name], before we get started, I wanted to see how you've been feeling overall since surgery. Have you noticed any changes in your appetite?"
- While cleaning the wound:"Protein is so important for your body to rebuild tissue. What are some protein sources you typically enjoy eating?"
- While applying a new dressing:Vitamin A helps your body build strong collagen and new skin cells to heal wounds faster. Foods like dark green leafy vegetables, sweet potatoes, carrots, squashes/pumpkins, mangoes, and papayas have vitamin A. Do you like any of those?
- Before wrapping up:" Providing our body with enough calories so it can heal is so important. Are you having any difficulty shopping for groceries or preparing meals?"
By incorporating these questions and discussions into your existing wound care routine, you can seamlessly integrate nutrition education into standard surgical follow-up procedures, promoting optimal wound healing for your patients.... and not taking up any more of your precious time! 😉
If you missed this episode, take a listen here.
What is the BEST diet for Prediabetes?
What the provider says: Hey Mr. Jeffers, your A1C was a little more elevated than we like to see. At 6.1% it puts you in the prediabetes range.
What the patient heard: "You have diabetes. You need to go on a diet."
The patient's immediate next question is, “Well, tell me what I can eat.”
I really wish it was that simple.
The high prevalence of prediabetes in the United States - affecting over 98 million adults - underscores the critical need for clear and empowering dietary guidance.
You remember the treatment for prediabetes that you learned in school, right? "Lifestyle modifications.” Easy. Exercise, weight loss, smoking cessation, physical activity....helpful for sure, but a little vague when you're staring at a real patient with real questions.
The truth is, the first line treatment for prediabetes is lifestyle modifications. But for our patients, that "lifestyle modification" prescription can feel about as clear as mud. So, let’s provide helpful guidance and empower our patients with prediabetes to take control of their health.
Here is a 5-step process to discussing prediabetes with patients
- Assess. What does the patient already know? “What do you know about prediabetes?” This respects their knowledge and gives you a baseline for where to go next in the conversation.
- Educate. Explain the disease simply. “Prediabetes is when your blood sugar is higher than normal, but not high enough for diabetes. The good news is, it’s reversible, but if left unchecked, can lead to several complications.” Understanding how food affects their blood sugar can improve their self-management.
- Ask. Find out what the patient’s diet looks like. “Can you tell me a little bit about your typical eating habits? How many times a day do you eat? What do you eat for breakfast, lunch, dinner? Do you usually snack between meals? If so, can you give me an example of what you might have? When it comes to drinks, what do you consume throughout the day?" This gives you an idea for areas of improvement.
- Present. Explain the principles of healthy eating for blood sugar control and the different dietary pattern options. “Prediabetes happens when your body struggles to use sugar or glucose for energy. Certain foods, especially those high in refined carbohydrates and sugar, can cause blood sugar spikes. This is why some dietary patterns can be very helpful in managing prediabetes. Here are a few options to consider: The Mediterranean Diet focuses on whole grains, fruits, vegetables, healthy fats like olive oil, and lean protein. It's known for its heart-healthy benefits and can also help with blood sugar control. The DASH Diet stands for Dietary Approaches to Stop Hypertension. It emphasizes fruits, vegetables, whole grains, and low-fat dairy products. It can help lower blood pressure and improve blood sugar management. The Diabetes Plate Method is a visual approach that uses a divided plate to guide portion control. Half the plate is filled with non-starchy vegetables, one quarter with lean protein, and the last quarter with whole grains or starchy vegetables. All these options are rich in fiber, which helps you feel fuller for longer and prevents blood sugar spikes. They also limit saturated fats and simple carbohydrates, which can contribute to blood sugar problems. We can discuss which approach might best fit your preferences and lifestyle."
- Collaborate. Allow the patient to consider what you said and choose a feasible change. This type of partnership works much better than you just giving them a diet to follow. “Knowing that you need to focus on your nutrition a bit more, what do you think you would like to work on first? Eating more fiber, drinking less sugar/tea or having less sweets? “
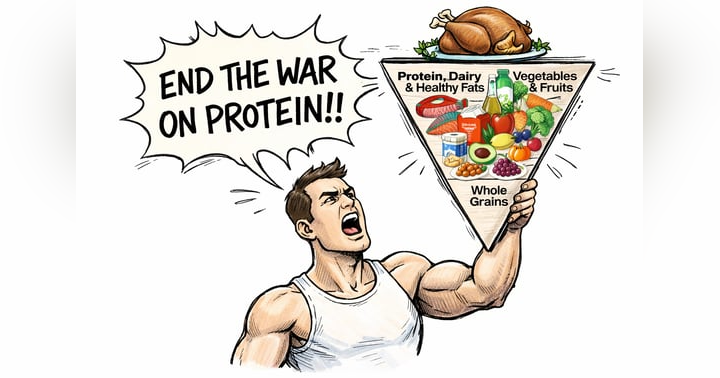
Now, let’s discuss which diet is best for prediabetes. Well, actually, no specific dietary pattern has proven to be superior over another. Reduction in A1C can be achieved through a variety of different eating patterns. Hence, why you shouldn’t just tell every patient to follow the DASH diet, when the Diabetes Plate Method might be more suitable for the patient’s lifestyle, preferences and schedule.
The key nutrition principles to focus on with your patients isn’t anything groundbreaking. Include non-starchy vegetables, whole fruits, legumes, whole grains, nuts/seeds, low-fat dairy, and minimal consumption of meat, sugar-sweetened drinks, sweets, refined grains, and ultra-processed foods. But this still feels overwhelming.
When I educate patients, I start with two areas: fiber and fluids!
- Fiber. If you focus your discussion on encouraging a high fiber diet, the patient will naturally begin following the above recommendations. Ideally ≥ 14 g fiber per 1,000 kcal, or roughly 25 grams for women and 38 grams for men (according to the USDA). Sources of fiber include vegetables, fruits, beans, lentils, chia seeds, whole grains (oats, barley, nuts/seeds, and avocado.
- Fluids. A simple change with a big reward is adjusting the beverages the patient consumes. Help them switch from high-sugar soda, fruit juice, tea and lemonade to water or fizzy water as much as possible.
Lastly, I will leave you with a list of unhelpful phrases to avoid. Although well-meaning, these are all confusing and unnecessary:
- “Watch your carbs”
- “Avoid all white foods”
- “No more sweets”
- “Just eat salad”
For a deeper discussion in pediatric prediabetes, check out this podcast episode: One Family, One Meal: Tackling Prediabetes Together
Your Questions, Answered
“My toddler won’t eat meat, I’m worried he’s not getting enough protein”
This is a very common concern in pediatrics. Reality is, a child doesn’t need as much protein as parents think.
A quick review for protein needs:
- 1–3 years: 13 grams per day
- 4–8 years: 19 grams per day
- 9–13 years: 34 grams per day
- 14–18 years: 52 grams per day for males and 46 grams per day for females
(These are general guidelines. A child may need more or less depending on medical conditions and physical activity.)
A common reason toddlers refuse meat could be texture. Toddlers are still developing their chewing skills, and meat might be difficult to manage.
If the child refuses meat, they can likely still meet their protein needs. For example, a toddler who drinks 1 cup of milk (8g protein), 1 cheese stick (5-6g protein), 1 scrambled egg (6g protein), 1 waffle (2g protein) comes to 21 grams, which is well above the 13 gram minimum for a toddler.
To ensure adequate protein and iron is met, be sure to ask if the child eats dairy foods, soy milk (similar nutrient content to dairy), beans, eggs, edamame or whole grains. These are all excellent sources of meat-free protein and iron.
In most cases, you can provide reassurance and help alleviate parental worry and encourage a balanced diet for their toddler.